Until recently, the model of what constitutes a companion diagnostic (CDx) for a drug was straightforward: It identified a biomarker that indicated an approved drug was indicated for a specific patient’s treatment. One test; one drug. It seems almost too elegant in its simplicity.
And often, it is. For patients with many forms of cancer, collecting an adequate quantity of tumor tissue for the test is often problematic, if not impossible, and in cases where a tissue samples is collected, a treating oncologist often needs to make an educated guess on which specific type of cancer to test for with a CDx. If the doctor’s educated guess for a patient is wrong the first time, then it’s back to another test if there is enough remaining tumor tissue. That’s a big if.
Today, as next-generation sequencing makes significant inroads for cancer diagnostics, the road map is changing. Multi-marker, pan-cancer CDxes leveraging the latest sequencing technologies are poised to significantly alter the landscape of one test for one drug, to one that allows for a single test to point toward many approved drugs.
Further, as significant effort and capital is expended to find the latest immunotherapies and combination therapies for cancer, the biomarker landscape is also changing. Where once pharma companies and their diagnostic partners searched for evidence of specific genetic variations, today their attention has turned to a new class of biomarkers and potential biomarkers such as PD-1, PD-L1, tumor mutational burden (TMB), and microsatellite instability (MSI) as researchers look to identify responders from non-responders of these new classes of very promising drugs.
“The drug companies and, obviously, the diagnostic companies are jumping on this as fast as they can. It is poised to really get traction because of the confluence of scientific and technical issues and also the growing commercial acceptance of next-generation sequencing as a valid cancer diagnostic test,” says David Parker, Ph.D., senior vice president, diagnostic solutions at Precision for Medicine. “It is when the commercial, the clinical, and the scientific all come together that the market really starts to move.”
PD-1 and PD-L1
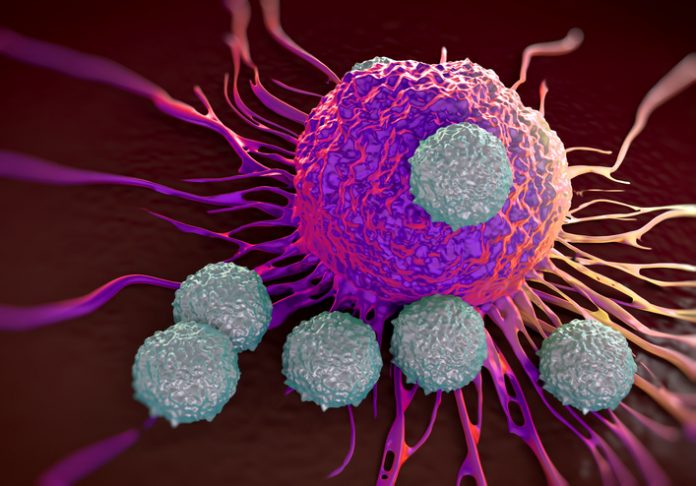
It’s not a stretch to say in the very early days of bringing immuno-oncology treatments to market, PD-1 and PD-L1 were the darlings of the dance. Overexpressed on tumor cells, PD-L1 binds to the PD-1 receptors on activated T cells, a clever biological trick that inhibits cytotoxic cells and with it, immune response.
As an immuno-oncology target, anti-PD-1 drugs have enjoyed significant success as evidenced by Bristol Myers Squibb’s approved drug nivolumab (Opdivo) and pembrolizumba (Keytruda) from Merck. Both drugs have added multiple FDA approvals for additional indications since first coming on the market for the treatment of metastatic melanoma, and advanced melanoma respectively.
Both the complementary diagnostics for nivolumab and the companion diagnostic for pembrolizumab followed a tried and true path for their pre-market approval.
“I suppose when we all entered the area of developing biomarkers for immuno-oncology, a lot of us had followed the traditional approach, which is you take the target which may be PD-1 or PD-L1 and you measure that, hopefully using immunohistochemistry. Then you look for a correlation for outcome,” says Richard Kennedy, Ph.D., global vice president of biomarker discovery with Almac Diagnostics. “That has been the model for a number of targeted biomarkers for a number of years, going back to HER2.”
While diagnostics based on these biomarkers continued to be employed and have even expanded their use for other indications (just before Clinical OMICs when to press, Agilent’s Dako PD-L1 IHC 22C3 pharmDx CDx for Keytruda received FDA approval for cervical cancer), over time PD-1 And PD-L1 have lost some of their luster.
One one hand, as researchers have delved deeper into biological mechanisms of the immune response to cancer, they have discovered other biomarkers that may more precisely predict response, such as tumor mutational burden (TMB) and microsatellite instability (MSI).
On the other hand, the testing methods and the related requirements for tissue needed for the tests may ultimately see their use limited.
In Parker’s opinion, scientists and clinicians may ultimately want more definitive answers. “The initial PD-1 an PD-L1 measurements are being made with immunohistochemistry, and generically immunohistochemistry is not a really great test,” Parker notes. “It is cumbersome to do, you need to have tissue samples, and it’s inherently a subjective measurement.
“In general, I think oncologists tend to prefer something that is a bit more definitive, and both mismatch repair and tumor mutational burden have the possibility of being much more objective tests.”
TMB and MSI
As the imperfections of PD-1 and PD-L1 have come to light and pharmaceutical companies and diagnostic makers look for potentially more precise biomarkers of I-O response or non-response, the road has led back to the tumor DNA to search for evidence of TMB and MSI.
In the case of TMB—a quantitative measure of the total number of mutations present per coding area of a tumor genome—there is growing evidence of its promise for companion diagnostics. Leading the pack is Bristol-Myers Squibb’s Phase 3 CheckMate -227 study of the combination therapy using two I-O agents, nivolumab and ipilimumab in advanced non-small cell lung cancer (NSCLC). In February, it released data that the study had met its primary endpoint of progression-free survival (PFS) of NSCLC patients whose tumor had high TMB regardless of PD-L1 expression.
“TMB has emerged as an important biomarker for the activity of immunotherapy. For the first time, this Phase 3 study shows superior PFS with first-line combination immunotherapy in a predefined population of NSCLC patients with high TMB,” said Matthew D. Hellmann, M.D., CheckMate-227 investigator and medical oncologist at Memorial Sloan Kettering Cancer Center, when the data were released. “CheckMate -227 showed that TMB is an important, independent predictive biomarker that can identify a population of first-line NSCLC patients who may benefit from the nivolumab plus ipilimumab combination.”
As Melanie Nallicheri, chief business officer of Foundation Medicine sees it, results such as those from CheckMate -227 point to TMB and MSI as important markers of I-O therapy response and also a path forward for the company’s FDA-approved FoundationOne CDx, a sequencing-based pan-cancer diagnostic that was used to measure TMB in the trial.
“We have a poster that shows the entire PD-L1 IHC universe and then shows the PD-1 positive patients and overlays that with those patients are who are tumor mutational burden high or microsatellite instability high,” Nallicheri says. “As you would surmise those that are tumor mutational burden high and MSI high is a smaller population but there is no full overlap between that population and those also having a PD-L1 positive status. So we have PD-L1 negative patients that may be tumor mutational burden high or MSI high in whom immunotherapy is indicated and you would want to treat them with immunotherapy.”
In the case of MSI, the biomarker has a longer track record than TMB, as it has been employed by pharmaceutical researchers as far back as the 1990s when mismatch repair was discovered as one of the major genetic abnormalities present in hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome. An indication of abnormal DNA repair in the mismatch repair pathway, the abnormal DNA that occurs from defective mismatch repair results in an immune response in tumors. MSI identifies this activity and patients characterized as MSI high typically won’t respond to anti-PD-L1 checkpoint blockade therapies.
For MSI research, Promega has provided the go-to PCR-based assay for much of the industry for years, but as the focus turns to the clinic for MSI, that platform of choice is migrating to panel-based, next-gen sequencing tests.
“I think the main drive for that is you get additional data,” notes Kennedy. “Using sequencing you can measure more than one thing. With a PCR assay, or an immunohistochemistry assay, it is a single test for a single biomarker. The issue for that is you use up a lot of tissue and if the assay is negative then what else are you going to do? You have no tissue to go back to. If you use a next-generation sequencing panel for MSI, you may be able to measure other assays using the same panel without going back and getting more tissue.”
Which is exactly the approach Foundation Medicine is taking with their CDx. It’s test not only queries more than 320 genes at one time, but can also simultaneously look for MSI and TMB. MSI, while more prevalent in Lynch syndrome or endometrial cancers, is much less common in others so being able to piggyback testing is both more time efficient and helps address the issue of depleting tumor tissue samples with multiple rounds of testing.
“We find that certain biomarkers are more prevalent than others in certain tissues or types of cancers,” Nallicheri says. “We have shown in the past that tumor mutational burden occurs across many cancers and colon cancers that are also MSI high, but it is not limited to those.”
Looking Ahead
While neither MSI or TMB are incorporated in an existing companion diagnostic today, that future doesn’t seem very far off. In late, May Merck tapped Foundation Medicine for the development of an MSI companion diagnostic for Keytruda.
“I think we will be seeing a next-generation sequencing-based companion diagnostic for MSI within the next two or three years, at most,” says Precision for Medicine’s Parker. In addition, he sees more work in TMB to potentially move it from a strictly quantitative measure of mutations, to using this information to better understand which mutations are important to disease pathology and which aren’t
“You don’t necessarily need to understand the biology of very single mutation,” he explains. “You just need to understand the ones that play a role in the disease.”
This would portend a greater role for next-generation sequencing tests and possibly even a move away from immunoassays and PCR for I-O diagnostics.
“We are hoping there will be broad acceptance by treating physicians that you need to leverage the tools that are at our disposal,” adds Nallicheri. “That means using next-generation sequencing based testing as opposed to relying on other methods of testing which are suboptimal for providing all of the information you could potentially have at your fingertips.”
The road ahead will likely bring other biomarkers to light, including additional protein biomarkers. According to Riley Ennis, chief operating officer for AI-driven diagnostics company Freenome, this approach would consider a broad range of analytes along with phenotypic information about patients that could paint a picture detailing a disease signature.
“I think there are other analytes in circulation and others ways of sequencing and applying machine learning to the problem to generate the data, but also to build a classifier for response prediction,” Ennis says. In addition, the company has begun working with companies that already have significant internal data and research on TMB and MSI, and are then looking to move one dimension beyond this information. A new CDx collaboration with Qiagen, announced in June, is an endorsement of the company’s approach.
“Some of the analytes people are looking at are relevant and have already been translated to clinical practice. The beauty of this is they are then giving us paired samples of TMB or MSI status and asking us to add that to one of our analytes,” he adds. Then we are looking empirically at what permutations or analytes work best independently, or in combination with each other, to maximize the sensitivity and specificity of predicting a cutoff of overall survival.”
And while not necessarily a mad scramble, Parker thinks the current market environment will spur the discovery of even more relevant biomarkers.
“The competition in the I-O space is so intense I would predict you are going to see every single player, both for mono therapy and combination therapy, eager to test every single biomarker advance that is offered by the diagnostic industry in the search for competitive advantage in the marketplace,” Parker concludes.






![AI Algorithm Could Reduce Breast Cancer Mammogram False Positive Rate The primary goal of the Paradigm Registry is to accelerate tumor profiling based on disease biology. [iStock/LilliDay]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/307-218x150.jpeg)




