Bristol Myers Squibb and bluebird bio’s autologous CAR T-cell therapy for multiple myeloma, idecabtagene vicleucel, succeeded in inducing at least a partial response in 73% of treated patients in a recent Phase II trial, with 33% having a complete response or achieving remission.
Multiple myeloma is a cancer of the white blood cells that is diagnosed in around 32,000 people per year in the U.S. Most treatments only induce responses in around a third of patients and long-term remissions are rare, with a five-year survival rate of around 54%.
In this study, which was published in the New England Journal of Medicine, 140 patients with relapsed and refractory myeloma who had undergone at least three previous treatment regimens were enrolled to trial idecabtagene vicleucel—‘ide-cel’. The trial was an international collaboration, but the main enrollment site was at the University of Texas Southwestern Medical Center.
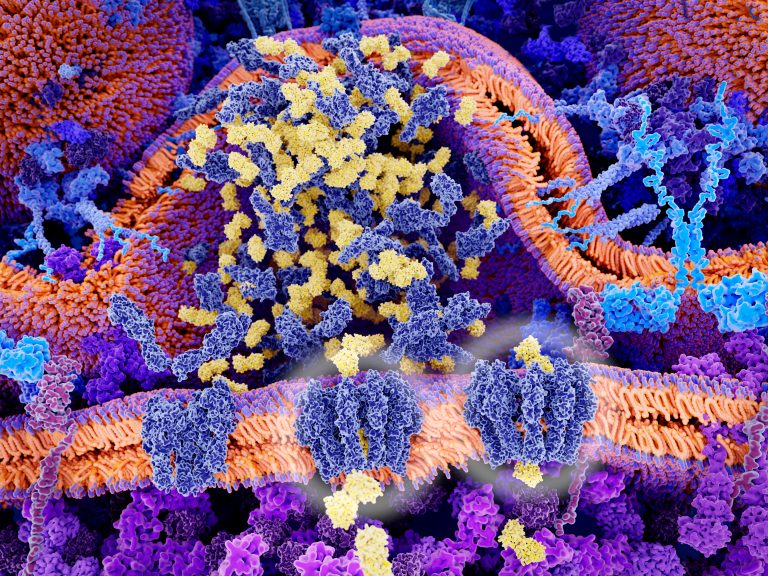
Overall, 128 patients received ide-cel. The therapy is autologous, which means that patients had their own T-cells extracted, and engineered to target B-cell maturation antigen, or BCMA, found in myeloma cells.
The trial’s primary endpoint was for at least 50% of patients to have a partial or greater response to the therapy. At 13.3 months, 94 (73%) of the patients had at least a partial response to the therapy and 42 (33%) had a complete response or had gone into remission.
Progression-free survival ranged from 5.6-11.6 months, with a median of 8.8 months. “We have patients that are over two years out from their single infusion of CAR T-cells and still in remission despite having no other treatment options when they were enrolled in this trial,” commented Larry Anderson Jr., M.D., Ph.D., an associate professor at the University of Texas and co-first author on the study.
“The results mark a true breakthrough with unprecedented depth and duration of remissions from what we hope will be the first cellular therapy option to become available for myeloma patients. Even though we don’t yet know if some of these patients may be cured, and many relapse within one to two years, it can at least buy many patients time until other treatment options become available.”
Side effects can be a big problem with CAR T-cell therapy. While they were observed on this study as well, the rate of severe side effects such as cytokine release syndrome or neutropenia of grade 3 or higher was relatively low at 3-5%.
“One of the nice things we saw in this study was that the rates of severe CAR T-cell-related toxicities – called neurotoxicity and cytokine release syndrome – were very low in multiple myeloma compared to what we have seen with lymphoma CAR T-cell infusions,” commented Anderson.
“The majority of people had some side effects, but most were low level and manageable, and I would say this therapy is often much better tolerated than a stem cell transplant, which most of these patients had already gone through.”
Currently, CAR T-cell therapies are only approved to treat leukemia and lymphoma. Based on the results of this trial, Bristol Myers Squibb and bluebird bio are now seeking FDA approval of ide-cel as a standard therapy for relapsed myeloma













