Immunotherapy has been a life-saving intervention for an array of diseases, particularly cancer. However, the treatments are not suited for every patient and can lead to serious side effects and even death. Understanding which patients would be best served by immunotherapy treatments is quickly becoming an essential factor in designing treatment strategies. As such, investigators at the Princess Margaret Cancer Centre in Toronto have discovered a gene signature biomarker that may predict which patients will respond—or not—to cancer immunotherapy.
Findings from the new study were published today in Nature Communications “TGF-β-associated extracellular matrix genes link cancer-associated fibroblasts to immune evasion and immunotherapy failure.”
“The extracellular matrix (ECM) gene signature associated with response to immune therapy is important because as of today we do not have a very good way to predict which patient will respond or which patient will not respond,” explains senior study investigator Daniel De Carvalho, Ph.D., senior scientist at Princess Margaret Cancer Centre.
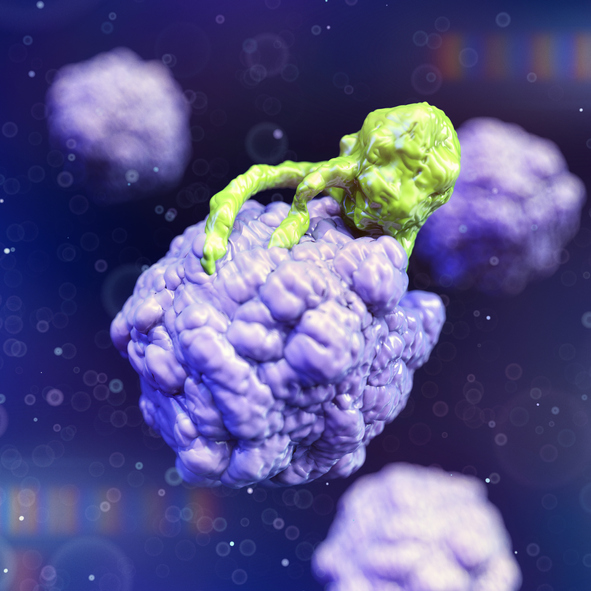
De Carvalho says the gene signature relates to the ECM, which underpins and physically supports cells. For cancer patients with the gene signature, the research suggests the ECM can stiffen around the diseased cells to form a barrier that immune cells simply cannot penetrate.
The multi-institutional scientific team used a big data approach and examined available data across thousands of patient samples from many different cancers to find that in some patients the immune cells were not penetrating the tumor, despite the fact these patients had molecular markers that would predict immune response.
“We reported findings from one of the largest pan-cancer analyses of ECM gene dysregulation in cancer. We defined a distinct set of ECM genes upregulated in cancer (C-ECM) and linked to worse prognosis,” the authors wrote. “We found that the C-ECM transcriptional program dysregulation is correlated with the activation of TGF-β signaling in cancer-associated fibroblasts and is linked to immunosuppression in otherwise immunologically active tumors. Cancers that activate this program carry distinct genomic profiles, such as BRAF, SMAD4, and TP53 mutations and MYC amplification. Finally, we showed that this signature is a predictor of the failure of the PD-1 blockade and outperforms previously-proposed biomarkers.”
With further experimental study to validate the biomarker, De Carvalho says the research lays the foundation for a new therapeutic strategy to focus first on ways to disable the ECM to enable immunotherapy.
“Our findings identify a distinct transcriptional pattern of ECM genes in operation across cancers that may be potentially targeted, pending preclinical validation, using the TGF-β blockade to enhance responses to the immune-checkpoint blockade,” the authors penned.
“The ultimate goal is to find a biomarker that can help the clinician decide if a patient should receive immunotherapy or not,” De Carvalho concluded. “Those who will not respond, the answer could be the patient would first receive a drug to target the ECM, and then be able to respond to immune therapy.”













