A blood test has been developed that allows detection and screening of Alzheimer’s disease (AD) for the first time, with an accuracy level of over 96%, according to a report from researchers at Hong Kong University of Science and Technology (HKUST).
“With the advancement of ultrasensitive blood-based protein detection technology, we have developed a simple, noninvasive, and accurate diagnostic solution for AD, which will greatly facilitate population-scale screening and staging of the disease,” said Nancy Ip, Morningside Professor of Life Science and the Director of the State Key Laboratory of Molecular Neuroscience at HKUST.
Described in a release as “The most comprehensive study of blood proteins in AD patients to date,” the work was published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
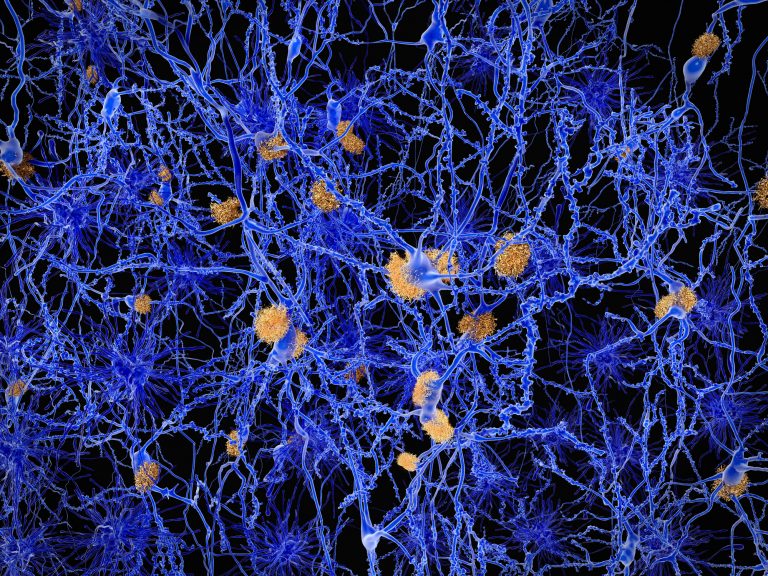
AD affects over 50 million people worldwide. It involves the dysfunction and loss of brain cells. Symptoms include progressive memory loss as well as impaired movement, reasoning, and judgment. While patients often only seek medical attention and are diagnosed when they have memory problems, AD affects the brain at least 10-20 years before symptoms appear.
Doctors mainly rely on cognitive tests to diagnose a person with AD. Besides clinical assessment, brain imaging and lumbar puncture are the two most commonly used medical procedures to detect changes in the brain caused by AD. However, these methods are expensive, invasive, and frequently unavailable in many countries.
The HKUST team, led by Nancy IP, Vice-President for Research and Development, has identified 19 out of the 429 plasma proteins associated with AD to form a biomarker panel representative of an “AD signature” in the blood. Based on this panel, the team has developed a scoring system that distinguishes AD patients from healthy people with more than 96% accuracy.
As the researchers note in their paper: “The recent discovery of blood-based AD biomarkers (i.e., plasma Aβ42/40 ratio, tau/phosphorylated tau [p-tau], and neurofilament light polypeptide [NfL]) raises the possibility of an alternative, less-invasive, blood-based test for AD.“ They note that, in particular, plasma p-tau181 and p-tau217 are believed to accurately classify AD.
Their process can also differentiate among the early, intermediate, and late stages of AD, and can be used to monitor the progression of the disease over time. Their findings have led to the development of a blood-based test for AD, and may also pave the way to novel therapeutic treatments for the disease.
The work was conducted in collaboration with researchers at University College London and clinicians in local hospitals including the Prince of Wales Hospital and Queen Elizabeth Hospital. The discovery was made using the proximity extension assay (PEA)—a high-throughput protein measurement technology, to examine the levels of over 1,000 proteins in the plasma.
PEA technology was used to evaluate the protein profiles of AD plasma in a Hong Kong Chinese AD cohort consisting of 106 patients with AD and 74 healthy controls (HCs) for whom demographic data, cognitive measures, brain region volumes, and plasma biomarker levels (i.e., Aβ42/40 ratio, tau, p-tau181, and NfL) were available.
The team then quantified 1160 plasma proteins and revealed 429 plasma dysregulatred proteins in patients with AD. According to their report, the researchers then identified a 19-protein biomarker panel representative of the plasma proteomic signature of AD and validated its high accuracy for classifying AD and associated endophenotypes in an independent cohort.











