Research carried out in mice shows that more than 200 gene variants help drive glioma formation with the help of the EGFR gene, dysfunction of which is implicated in several cancers.
An international team of scientists, based mostly at the Wellcome Trust Sanger Institute and the University of Cambridge in the UK, created an EGFR-mutant mouse model of glioma to help researchers searching for new drug targets for these cancers.
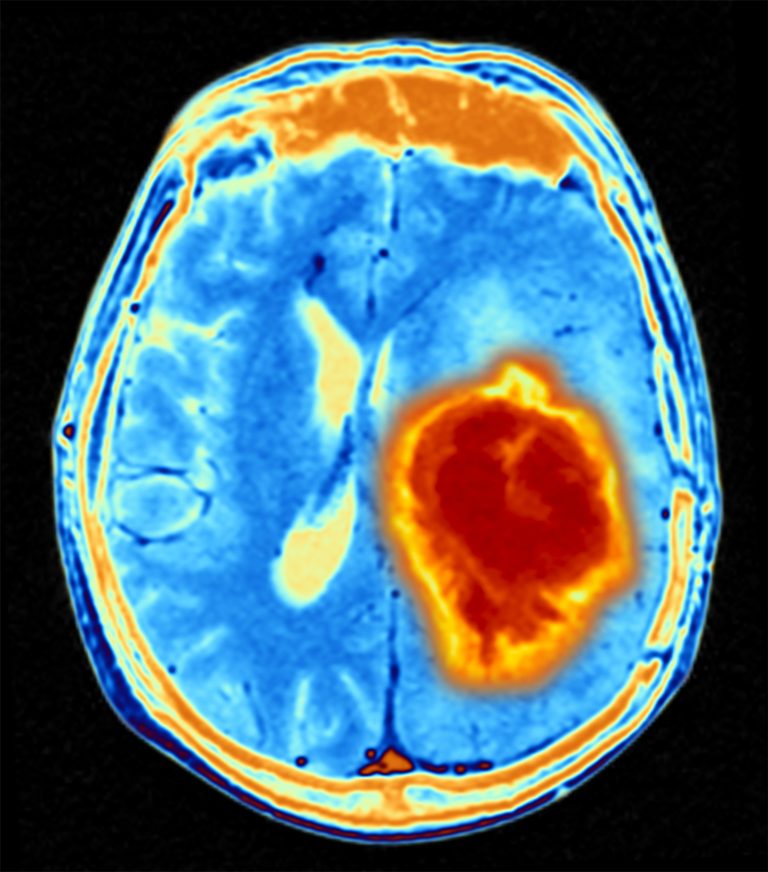
Glioma accounts for around 30% of all brain and spinal tumors. Grade IV glioma, or glioblastoma, is an aggressive brain cancer, with a very low survival rate and new, more effective treatments are desperately needed.
It is known that the majority of glioblastoma’s have mutations in the EGFR gene, but until now it has not been totally clear what causes the cancer to start and what role mutations in other genes, such as those that normally suppress tumor formation, play in driving this cancer.
As reported in the journal Genome Biology, the research team found that a specific mutation in the EGFR gene alone was enough to trigger development of a mouse version of glioblastoma that showed strong similarities to the human cancer.
They also used a technique known as the ‘PiggyBac transposon’ method, which involves inserting small sections of DNA around the genome in the mice. Via this technique they found more than 250 mutations in tumor suppressor and oncogenes that aided the development of gliomas in the animals.
“For the first time, we showed that the familiar cancer gene, EGFR is capable of initiating glioblastoma and we identified new driver genes, whose potential for therapeutic targeting deserves further exploration,” said Imran Noorani, MD, first author on the paper, a researcher from Addenbrooke’s Hospital and the University of Cambridge.
To confirm these mutations were also linked to gliomas in humans, the team tested samples from people with both low grade glioma and glioblastoma and found significant correlation with the mouse model, validating its use for testing potential drugs for the cancer in the future.
“Glioblastoma patients urgently require new, targeted therapies,” emphasized Allan Bradley, PhD, Chief Scientific Officer at Kymab and formerly Director of the Sanger Institute, who was a senior author on the study.
“Unfortunately, glioblastoma tumours can become highly resistant to therapies that target specific molecules, as there are many other genetic drivers that can ‘take over’ progressing the cancer. This new mouse model provides the missing link to translate findings from new potential treatments tested on mice to clinical trials.”
Although further research is needed, the scientists did some initial drug exposure testing and believe many of the driver mutations they discovered could be druggable, which gives hope for glioma and glioblastoma patients in the future.













