Disabling immune suppression mediated by a specific type of macrophage may boost the effectiveness of poly ADP ribose polymerase (PARP) inhibitor therapy for some forms of breast cancer, according to research lead by a team of investigators from the Dana-Farber Cancer Institute (DFCI).
Reporting in Nature Cancer, the researchers identified macrophage-mediated immune suppression as a weak spot of PARP inhibition treatment, and indicated that combining PARP inhibitor therapy with an anti-colony-stimulating factor 1 receptor (CSF1R) therapy could boost therapeutic efficacy against BRCA-associated triple-negative breast cancer (TNBC).
Reporting their findings in a paper titled, “Targeting immunosuppressive macrophages overcomes PARP inhibitor resistance in BRCA1-associated triple-negative breast cancer,” the team concluded: “Collectively, our results uncover macrophage-mediated immune suppression as a liability of PARP inhibitor treatment and demonstrate that combined PARP inhibition and macrophage-targeting therapy induces a durable reprogramming of the tumor microenvironment (TME), thus constituting a promising therapeutic strategy for TNBC.”
Breast cancer is the second most common cancer in the United States, and can be associated with mutations in the DNA-repairing breast cancer gene, BRCA. “Mutations in BRCA genes render cells susceptible to chromosomal instability through defective DNA strand break repair, leading to increased risk of breast cancer,” the team explained. Typically, BRCA-associated breast cancer is treated using PARP inhibitors and, recently, clinical trials have investigated pairing PARP inhibitor therapy with immunotherapy. Based on preclinical data, it is expected that the combination will recruit and activate immune system tumor-killing T cells. Initial results of the combination of a PARP inhibitor and a checkpoint inhibitor in small numbers of patients with metastatic breast cancer have shown this combination to be active, the researchers indicated, and a national pre-surgical trial led by DFCI investigators has recently opened and will examine this targeted combination in patients with genetic mutations sensitive to PARP inhibitors.
Given the clinical potential of this treatment combination, researchers are already looking for ways to get even more benefit from PARP inhibitors plus checkpoint inhibitors in breast cancer patients. The Dana-Farber/Brigham and Women’s Cancer Center team has focused research on identifying ways to boost the response to PARP inhibitors. “The question that drove our research was: How can we overcome PARP inhibitor resistance to turn this treatment into a home run?” said Jennifer Guerriero, Ph.D., senior author and member of the Brigham’s Division of Breast Surgery and director of the Dana-Farber Breast Tumor Immunology Laboratory. “Our findings suggest that there’s something in the tumor microenvironment limiting the ability for T cells to be activated, and that something else is likely macrophages, which we found become highly suppressive after PARP inhibitor therapy.”
Similar to BRCA proteins, PARP proteins act to repair damaged DNA. In tumors, inhibiting DNA repair can lead to cancer cell death, so the combined elimination of BRCA and PARP repair mechanisms induce cancer cell death. PARP inhibitors also recruit T cells, which are required for the body to recognize the presence of cancerous cells.
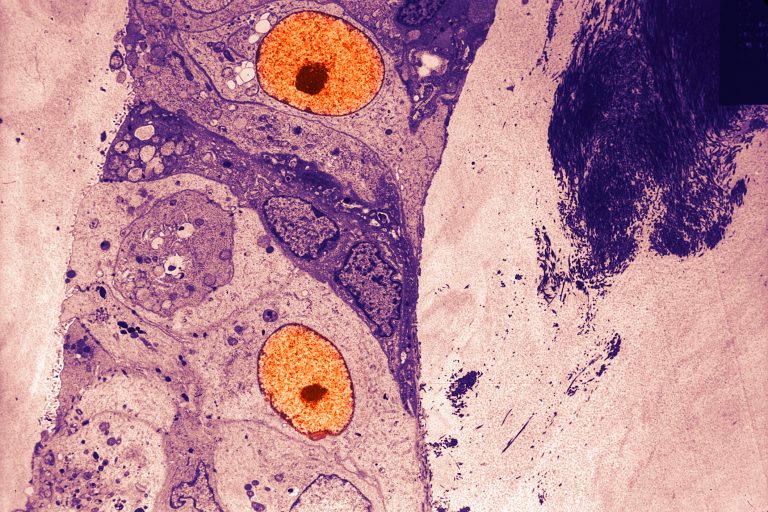
Like T cells, macrophages are a type of immune cell, and are recruited to wounds to patch them up. In cancer, which is viewed as wounds to macrophages, these cells are recruited to tumor sites, and repair, strengthen, and, consequentially, exacerbate the tumor state. The team’s experiments showed that in BRCA-associated TNBC, PARP inhibitor treatment leads to increased numbers of macrophages being recruited to the tumor site. “Here, we mechanistically dissected the TME of human BRCA-associated TNBC using high-dimensional single-cell profiling to reveal that BRCA-associated TNBC has significantly more macrophages than BRCA-proficient TNBC …” they noted. “Extensive characterization of tumor macrophages in a mouse model of BRCA1-deficient TNBC revealed that macrophages numbers increase further after PARP inhibitor treatment and have both pro- and antitumor phenotypes.”
Further analysis showed a particular abundance of macrophages expressing a receptor, CSF1R, which is necessary for their survival, in cancerous tissue after PARP inhibition treatment. Given this observation, the researchers hypothesized that targeting CSF-1R-positive macrophages—a particularly suppressive macrophage type—in combination with PARP inhibition would lead to an enhanced antitumor response.
Since CSF1R-positive macrophages exacerbate the tumor state, the team focused on disabling these macrophages. Using the TNBC BRCA-deficient mouse model, the team characterized these suppressive macrophages by assessing T cell and macrophage responses to different therapies and combinations of therapies.
They found that therapy using the PARP inhibitor olaparib in combination with a CSF1R inhibitor resulted in dramatic antitumor responses and significant increase in overall survival. “Combining PARP inhibitor therapy with CSF1R-blocking antibodies significantly enhanced innate and adaptive antitumor immunity and extended survival in mice with BRCA-deficient tumors in vivo, and this was mediated by CD8+ T cells,” they commented.
Furthermore, the triple combination of PARP inhibitor, CSF1R inhibitor, and inhibition of SREBP1 (a key regulator of lipid metabolism) was able to completely eliminate tumors in the aggressive TNBC mouse model. Researchers inferred from this therapeutic success that the PARP inhibitor directly activates macrophages to be suppressive in the tumor microenvironment. “Here we provide evidence that olaparib can modulate the maturation, phenotype, function, and metabolic state of macrophages through PARP1-independent and -dependent pathways, which can be reversed by inhibiting SREBP1,” the team noted.
While breast cancer tissue is often characterized before treatment, taking biopsies of tissue after treatment has started could provide further insight into the cell types present. As the authors concluded, “We provide evidence that PARP inhibition can modulate macrophage state, phenotype, function, and metabolism. In addition, we show that PARP inhibition increases the expression of CSF1R in differentiating macrophages, providing a rationale for the combination of anti-CSF1R and PARP inhibitor therapy to reduce pro-tumor macrophages, resulting in activation of antitumor macrophages and CD8+ T cells and induction of long-term antitumor immunity to overcome PARP inhibitor resistance.” Importantly, elucidating PARP- and macrophage-mediated mechanisms will be critical in developing effective therapies and moving forward with clinical translation.
“At Dana-Farber/Brigham and Women’s Cancer Center we have the opportunity to work closely with our clinical colleagues and ask these really important questions that will be critical to identify better biomarkers, so we can identify which patients will respond to which therapies,” said Guerriero. “I am very optimistic about the use of PARP inhibitors—they are a game-changer for patients with BRCA-deficient cancers, and their application is not just limited to breast cancers.”













