Blood levels of neurofilament light chain (NfL) are a useful biomarker of neurodegenerative diseases such as Down’s syndrome dementia, motor neuron disease (ALS), and frontotemporal dementia, even without definitive clinical symptoms, a new study finds. Further, this research determined a set of age-related cut-off levels of NfL which could help in the design of a diagnostic.
“For the first time we have shown across a number of disorders that a single biomarker can indicate the presence of underlying neurodegeneration with excellent accuracy. Though it is not specific for any one disorder, it could help in services such as memory clinics as a rapid screening tool to identify whether memory, thinking or psychiatric problems are a result of neurodegeneration,” said joint senior researcher on the study, Abdul Hye, Ph.D., from the NIHR Maudsley Biomedical Research Centre at King’s College London.
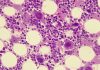
It’s estimated that there are approximately 50 million people worldwide suffering from dementia. Current biomarkers for neurodegenerative disorders are taken from cerebrospinal fluid (CSF), which has to be extracted using lumbar puncture. But a central and irreversible feature in many neurodegenerative disorders is damage to the nerve fiber. That results in the release of NfL, which can be detected in blood even at low levels. NfL is increased in a number of neurodegenerative disorders.
The study, published in Nature Communications today, analyzed 3138 samples from King’s College London, Lund University, and Alzheimer’s Disease Neuroimaging Initiative, including people with no cognitive impairment, with neurodegenerative disorders, with Down syndrome, and with depression.
Concentrations of NfL in the blood were higher across all neurodegenerative disorders compared to those in people with no cognitive problems. The highest levels were seen in people with Down’s syndrome dementia, motor neuron disease, and frontotemporal dementia.
The study also showed that although blood based NfL levels did not differentiate between disorders, it could provide insight into different groups within certain disorders. For example, in those with Parkinson’s a high concentration of NfL indicated atypical Parkinson’s disorder, and in patients with Down syndrome NfL levels differentiated between those with and without dementia.
“For neurodegenerative diseases like Alzheimer’s, Parkinson’s or motor neuron disease, a blood test to allow early diagnosis and help us monitor disease progression and response to treatment would be very helpful. Neurofilament light chain is a promising biomarker that could speed diagnosis of neurodegenerative diseases and shorten clinical trials,” said co-author Ammar Al-Chalabi, M.D., Ph.D., a professor from King’s College London and co-lead of the Psychosis and Neuropsychiatry research theme at the NIHR Maudsley BRC.
The study assessed age-related thresholds or cut-offs of NfL concentrations that could represent the point at which an individual would receive a diagnosis. These age-related cut-off points were 90% accurate in highlighting neurodegeneration in those over 65 years of age and 100% accurate in detecting motor neuron disease and Down syndrome dementia in the King’s College London samples, with a very similar result in the Lund samples.
Importantly, NfL was able to distinguish individuals with depression from individuals with neurodegenerative disorders that commonly present with primary psychiatric disorder in the onset of disease development such as frontotemporal dementia.
Joint senior author Oskar Hansson from Lund University said, “Blood tests have great potential to improve the diagnosis of dementia both in specialized memory clinics and in primary care. Plasma NfL can be extremely useful in a number of clinical scenarios which can greatly inform doctors, as shown in this large study.”