A drug that is currently prescribed to treat a rare enzyme deficiency can help cells to clear herpes simplex 1 (HSV-1) and herpes simplex 2 (HSV-2) viruses, according to researchers at the University of Illinois at Chicago (UIC). In vitro and in vivo studies, reported in Science Advances, demonstrated that antiviral activity of the drug, phenylbutyrate (PBA), was even better when used in combination with acyclovir, a common treatment for HSV-1 treatment. Adding PBA to acyclovir therapy meant that less acyclovir was needed to effectively suppress the virus. This was a significant finding, the researchers suggested, as acyclovir can have toxic side effects in the kidneys.
“There are very few drugs available to treat herpes simplex viruses, so when new drugs become available, especially drugs that enable fewer side effects, it is a welcome discovery,” said Deepak Shukla, PhD, the Marion Schenk professor of ophthalmology and UIC professor of microbiology and immunology at the College of Medicine. “Acyclovir can have very toxic effects on the kidneys, especially when it is given in higher doses for HSV-induced encephalitis, which is rare but can be deadly. By combining acyclovir with PBA, we need less acyclovir to effectively treat HSV-1.” Shukla is corresponding author of the team’s paper, which is titled, “Standalone or combinatorial phenylbutyrate therapy shows excellent antiviral activity and mimics CREB3 silencing.”
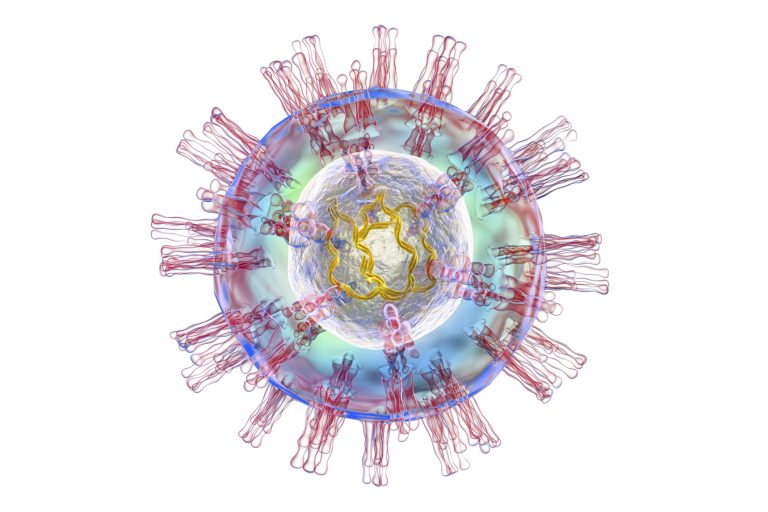
There are two types of herpes simplex virus that infect humans. Herpes simplex 1 infects the eyes and mouth, and is a leading cause of blindness. Herpes simplex 2 manifests as a genital infection that may cause painful sores and can seriously impair quality of life. Treatment for both infections often includes systemic use of the drug acyclovir, which is given orally. However, long-term use of the drug can lead to treatment resistance, as well as kidney damage.
Herpes viruses tightly regulate many cellular pathways, including the unfolded protein response (UPR), an important mechanism that is initiated as a result of endoplasmic reticulum (ER) stress, the authors wrote. ER stress is caused by the accumulation of misfolded, unfolded proteins in the ER. Host cells infected with viruses are triggered to produce viral proteins so that the virus can replicate itself. But the cells also continue to produce proteins for their own use, leading to ER stress. “ER stress is one of the main stress pathways that the virus uses to regulate its replication inside a host cell,” the team continued. “It does so by controlling important ER membrane proteins to its own advantage …” Previous studies have shown that HSV “effectively disarms the UPR,” while producing, folding, and secreting viral proteins from the ER without triggering cell death pathways.
“This robust modulation of UPR by the virus has intrigued the interest of herpes virologists to uncover underlying mechanisms that can be exploited to control virus replication,” the investigators continued. Scientists have in particular been interested in a protein known as CREB3, which has been “… in the spotlight …” as a homolog of an HSV-1 protein known as VP16, both of which can bind to host cell factors to trigger transcription of certain HSV genes. However, the authors acknowledged, “While the role of CREB3 in the host and during HSV infection has been extensively hypothesized, no evidence currently exists that conclusively details its role in primary infection.”
For their reported studies, Shukla and colleagues investigated the effects of PBA—a chemical chaperone–based alleviator of ER stress, which is used to treat certain urea cycle disorders—on HSV type 1 infection. “ … this study focuses on the importance of CREB3 as a prosurvival, proviral factor that HSV uses for its own benefit.” Their in vitro experiments found that PBA disrupts the ability of HSV-1 to hijack the cellular machinery that is used to produce proteins. Treating HSV-infected cells using PBA effectively down-regulated the ER-localized host protein CREB3, resulting in inhibition of viral protein synthesis.
The experiments further showed that PBA alone was as effective as acyclovir in its ability to clear HSV-1 from cells of donated human corneas or from donated human skin tissue. The drug was also effective against HSV in live mice. In a mouse model of ocular HSV-1 infection, PBA administered intraperitoneally was able to clear the virus from the eyes. And in a mouse model of HSV-2 vaginal infection, animals that received PBA had no signs of the HSV-2 virus in tissues, similar to mice treated with acyclovir. “Using several different in vitro, ex vivo, and animal models of infection, we found that PBA was highly effective in reducing HSV infection, and the levels of antiviral activity were similar to a currently prescribed antiviral for human HSV infections,” the scientists commented. “At its therapeutic concentration, we show that PBA regulates ER stress without any adverse toxicity to cells.”
“We found that PBA reduces stress on the ER, which allows the cell to focus on clearing the virus on its own,” said first author Tejabhiram Yadavalli, PhD, a UIC ophthalmology and visual sciences postdoctoral fellow.
Tests with a combination of PBA and acyclovir in cells infected with HSV-1 also confirmed that the dual therapy was able to completely clear the virus faster and better than either drug alone. Additionally, experiments in a mouse model of HSV-induced encephalitis showed that while animals treated with PBA or acyclovir alone had significantly reduced death rates, a combination of PBA and acyclovir was able to prevent death in all treated mice. The researchers said their results indicated that clinical trials with PBA may be warranted. “ … pharmacological mimicry of CREB3 silencing using an FDA-approved drug such as PBA can work as an excellent strategy to inhibit HSV infections .… we propose that this drug can provide an alternative to current antivirals to treat both ocular HSV-1 and genital HSV-2 infections and may be a strong candidate for human trials,” they wrote.
“PBA is an exciting new therapeutic for treating herpes infections that can help reduce side effects associated with long term or high dose use of acyclovir, a commonly prescribed medication to treat herpes viruses,” Shukla said. “The added bonus of this drug already being approved by the FDA to treat a rare enzyme disorder means that we may be able to quickly develop a marketable new combination therapy in the near future.”






![AI Algorithm Could Reduce Breast Cancer Mammogram False Positive Rate The primary goal of the Paradigm Registry is to accelerate tumor profiling based on disease biology. [iStock/LilliDay]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/307-218x150.jpeg)






