The results of a small-scale study in human volunteers have shown how specifically low-carb, high-fat ketogenic diets (KDs)—which are widely publicized for their purported health and weight loss-promoting benefits—have a dramatic impact on the gut microbiome that differs to that of high-fat diets (HFDs). Additional studies in mice by the same University of California, San Francisco (UCSF)-led research team demonstrated that ketone bodies, which are a molecular byproduct that gives the ketogenic diet its name, directly change levels of certain types of gut bacteria, which led to reduced levels of intestinal pro-inflammatory immune cells. They suggest the results provide initial evidence for the potential benefits of ketone bodies as a therapy for autoimmune disorders affecting the gut.
“This is a really fascinating finding because it suggests that the effects of ketogenic diets on the microbiome are not just about the diet itself, but how the diet alters the body’s metabolism, which then has downstream effects on the microbiome,” said Peter Turnbaugh, PhD, a UCSF associate professor of microbiology and immunology, member of the UCSF Benioff Center for Microbiome Medicine, and a Chan Zuckerberg Biohub investigator. “For many people, maintaining a strict low-carbohydrate or ketogenic diet is extremely challenging, but if future studies find that there are health benefits from the microbial shifts caused by ketone bodies themselves, that could make for a much more palatable therapeutic approach.”
Turnbaugh and colleagues report on their studies in Cell, in a paper titled, “Ketogenic Diets Alter the Gut Microbiome Resulting in Decreased Intestinal Th17 Cells.”
A ketogenic diet involves dramatically reducing carbohydrate consumption in order to force the body to alter its metabolism to using fat molecules rather than carbohydrates as its primary energy source, and producing ketone bodies as a byproduct. This shift in metabolism is claimed by some to have numerous health benefits, but, as the authors noted, while such diets are used for multiple diseases, “their metabolic and immune consequences remain unclear.”
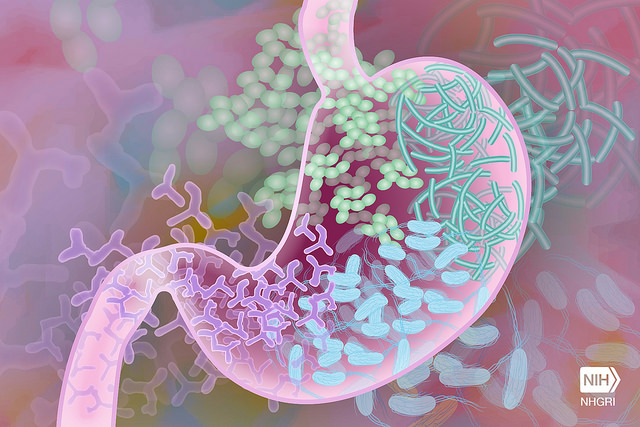
One possibility is that KDs might impact on gut microbiota. “I got interested in this question because our prior research showed that high-fat diets induce shifts in the gut microbiome that promote metabolic and other diseases in mice, yet ketogenic diets, which are even higher in fat content, have been proposed as a way to prevent or even treat disease,” said Turnbaugh. “We decided to explore that puzzling dichotomy.”
For their newly reported study, the UCSF-led team partnered with the nonprofit Nutrition Science Initiative to recruit 17 adult overweight or obese nondiabetic men to spend two months as inpatients in a metabolic ward where their diets and exercise levels were carefully monitored and controlled. For the first four weeks of the study, the participants were given either a standard diet consisting of 50% carbohydrates, 15% protein, and 35% fat, or a ketogenic diet comprising 5% carbohydrates, 15% protein, and 80% fat. After four weeks, the two groups switched diets, to allow the researchers to study how shifting between the two diets altered participants’ microbiomes.
Analysis of microbial DNA in the participants’ stool samples showed that shifting between standard and ketogenic diets dramatically changed the proportions of common gut microbial phyla Actinobacteria, Bacteroidetes, and Firmicutes, including significant changes in 19 different bacterial genera. The researchers focused on a particular bacterial genus— the common probiotic Bifidobacteria—which showed the greatest decrease in individuals on the ketogenic diet.
To better understand how microbial shifts on the ketogenic diet might impact health, the researchers turned to mice, and exposed the mouse gut to different components of the microbiomes of humans adhering to ketogenic diets. Their results showed that these altered microbial populations specifically reduced the numbers of Th17 immune cells, a type of T cell that is critical for fighting off infectious disease, but which is also known to promote inflammation in autoimmune diseases.
Follow-up experiments in mice, in which researchers gradually shifted animals’ diets between low-fat, high-fat, and low-carbohydrate ketogenic diets, confirmed that high-fat and ketogenic diets have opposite effects on the gut microbiome. These findings suggested that the microbiome responds differently as the level of fat in the animals’ diet increases to levels that promote ketone body production in the absence of carbs.
The researchers observed that that as animals’ diets were shifted from a standard diet towards stricter carbohydrate restriction, there was a shift in microbial populations that correlated with a gradual rise in ketone bodies. “Circulating ketone body levels increased as dietary CHO decreased,” they wrote.
“This was a little surprising to me,” Turnbaugh said. “As someone who is new to the keto field, I had assumed that producing ketone bodies was an all-or-nothing effect once you got to a low enough level of carb intake. But this suggests that you may get some of the effects of ketosis quite quickly.”
The researchers tested whether directly feeding ketone bodies to mice could drive the microbial shifts they had seen in the gut’s microbial ecosystem, without changing the animals’ diets. They found that even in mice who were eating normal amounts of carbohydrates, the presence of added ketones was enough to produce many of the specific microbial changes seen when they were consuming the ketogenic diet.
The combined results suggest that diet-induced changes in host metabolites alter the gut microbiota, which has downstream effects on immune cells, the team suggested. The impact of a ketogenic diet on the gut microbiota is distinctive from that of an HFD, due in part to the concomitant host production of ketone bodies. “Inhibition of bifidobacterial growth by ketone bodies results in KD-associated decreases in intestinal Th17 cell levels and possibly also adipose tissues,” they concluded. “Given the links between obesity and chronic low-grade inflammation, decreased levels of pro-inflammatory Th17 cells in both gut and adipose tissues on a KD may be a potential mechanism contributing to the greater efficacy of KD in improving some aspects of metabolic syndrome such as glycemic control and reductions in body fat.”
The scientists say their results provide a rationale for further research into the potential role that Th17 immune responses might play in the effectiveness of KD as a treatment for diseases such as refractory epilepsy, and potentially other diseases, including autoimmune disorders, which are associated with increased Th17 cells. As they pointed out, “Aside from reported metabolic effects in clinical trials, KDs have been used as dietary treatment for intractable epilepsy since the 1920s and recent studies have found significantly positive outcomes with the use of KDs for treatment of refractory epilepsy in children and adults where anti-epileptic drugs have failed.”
While they acknowledged that more work will be needed to better understand the long-term consequences of KD on health and disease, the reported study “highlights the role of the gut microbiota in mediating changes in intestinal Th17 cell responses to KD consumption,” they concluded. “Overall, this work extends important previous findings from our laboratory and others, providing evidence that the impact of diet on the gut microbiota is not only translatable from animal models to humans, but also appears to play a causal role in mediating host immune responses to diet. Continued progress in elucidating the mechanistic basis for these observations could help inform more personalized approaches to utilize dietary interventions for the prevention and treatment of human diseases.”
Co-authors John Newman PhD, and Eric Verdin, PhD, at the Buck Institute for Research on Aging, are co-founders with equity interest of BHB Therapeutics, which is developing products related to ketone bodies.













